Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
At Kanaa Fertility Centre, is performed by highly experienced specialists using the latest microsurgical techniques and equipment to diagnose and treat male infertility. This minimally invasive procedure has proven successful in modern fertility care, offering men a safe and effective option to retrieve sperm for IVF or ICSI, with precision and minimal discomfort.
Sperm retrieval procedures are medical techniques used to collect sperm directly from the testes or epididymis when sperm is not present in the ejaculate. These procedures are commonly recommended for men with azoospermia, severe male infertility, or ejaculation issues and are usually performed as part of IVF with ICSI.
Male infertility can sometimes prevent sperm from being present in the semen, even when sperm production is occurring inside the testes. In such cases, sperm retrieval procedures make it possible to collect sperm directly from the reproductive tract and use it for assisted fertility treatment.
Sperm retrieval plays a critical role in modern fertility treatments, allowing many men with severe infertility to achieve biological parenthood through IVF treatment and ICSI treatment.
This page explains what sperm retrieval procedures are, when they are needed, the different types available, how they work, and what couples can expect before and after the procedure.
Sperm retrieval procedures are minor surgical or minimally invasive techniques used to obtain sperm directly from:
Retrieved sperm is typically used with ICSI treatment, where a single sperm is injected directly into an egg during IVF.
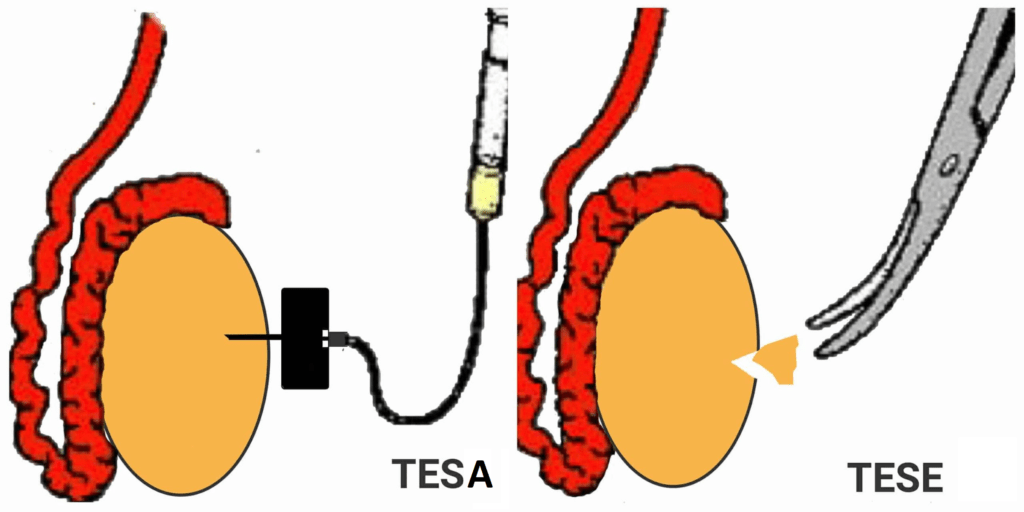
Men who have male factor infertility will sometimes produce semen with no sperm, also known as azoospermia. But couples struggling with male factor infertility still have options. In the past, the only options for treating azoospermia were reconstructive surgery (if there was obstruction) or donor insemination. Now intra-cytoplasmic sperm injection (ICSI) has enabled many azoospermic men to become biological fathers using sperm obtained from their epididymis or testis. Two of the most common sperm retrieval procedures are Testicular Sperm Aspiration (TESA) and Testicular Sperm Extraction (TESE). Couples should understand the difference between TESA and TESE and discuss their best treatment options with their physician.
Procedure:
TESA is a procedure that can be performed in the clinic. In TESA, one or both of the testes are numbed, and then the physician uses a needle to aspirate sperm. This means that the physician obtains a small sample of tissue using gentle suction to examine under a microscope. If the tissue sample shows adequate amounts of sperm, the physician then takes another small tissue sample for sperm extraction.
In TESE, the physician performs a surgical biopsy of the testis to retrieve tissue that contains sperm. Usually, this tissue has already been identified through mapping techniques and then, through a small incision, is extracted.
TESE Procedure
Surgical testicular biopsy to retrieve tissue with sperm, usually applied if TESA is insufficient.
Doctors may recommend sperm retrieval in the following situations:
Azoospermia (No sperm in semen)
When semen analysis shows no sperm, sperm retrieval may help identify viable sperm inside the testes or epididymis.
Obstructive azoospermia
When sperm production is normal but blocked due to:
Non-obstructive azoospermia
When sperm production is reduced but small numbers of sperm may still be present in the testes.
Ejaculation disorders
Conditions where sperm cannot be ejaculated normally due to nerve damage or medical conditions.
Severe male infertility
When ejaculated sperm quality is extremely poor and direct retrieval offers better fertilization potential.
The choice of procedure depends on diagnosis, test results, and fertility goals.
This method may improve sperm retrieval success in complex cases.
Doctors perform:
Retrieved sperm is immediately examined in the lab. Viable sperm may be:
Most men experience mild discomfort or swelling for a short period. Recovery is usually quick with simple precautions.
Retrieved sperm is almost always used with ICSI treatment because:
ICSI allows fertilization even with very few sperm.
Outcomes depend on:
Obstructive azoospermia generally has higher retrieval success than non-obstructive.
Presence of sperm-producing tissue influences success.
Advanced embryology labs improve fertilization outcomes.
Egg quality and uterine health also affect pregnancy outcomes.
Aspect | Sperm Retrieval | Donor Sperm |
Genetic link | Yes | No |
Medical complexity | Higher | Lower |
Fertility method | IVF + ICSI | IUI / IVF |
Used when | Own sperm possible | No viable sperm |
Doctors help couples choose the most appropriate option based on medical findings.
Sperm retrieval procedures are generally safe when performed by experienced specialists. Possible risks include:
Doctors provide aftercare instructions to minimize risks.
Male infertility can be emotionally challenging. Sperm retrieval often offers hope where natural conception was not possible.
Clear counselling and supportive care help patients navigate this process confidently.
Sperm retrieval procedures provide an effective fertility option for men with severe infertility or absence of sperm in the ejaculate. By directly obtaining sperm from the testes or epididymis, these techniques make biological parenthood possible through IVF and ICSI.
A fertility specialist can determine the most appropriate retrieval method based on semen analysis, hormonal evaluation, and overall fertility assessment.
TESA is most appropriate for men who have an adequate amount of sperm throughout the testicles. Occasionally, TESA doesn’t provide enough tissue/sperm and an open testis biopsy is needed.
TESE is one of the best ways to find sperm that a couple can use for ICSI or IVF procedures. The goals of TESE are to extract as much usable sperm as possible so that the couple have an adequate amount to fertilize an egg. TESE also minimizes any damage to reproductive organs and is usually done under local anesthesia to decrease pain or discomfort. TESE is sometimes done diagnostically to find out if a man has enough sperm. It may also be appropriate for men who are producing sperm, but are not candidates for other procedures because of scar tissue or prior surgeries.
After a man undergoes sperm extraction through TESA or TESE, he may feel some discomfort for a few days. Usually, he can resume non-vigorous activity after 2-3 days. There may be some swelling, bruising, or small amounts of fluid drainage for a few days. Following TESA or TESE procedures, men can take over-the-counter pain medications, and should emphasize rest and a healthy diet.
Sperm retrieval refers to different medical procedures used to collect sperm directly from the male reproductive system when it is not present in the semen. It is commonly used in IVF or ICSI treatments.
It is recommended for men with:
Blockages in the reproductive tract (obstructive azoospermia)
Very low or no sperm in the semen (non-obstructive azoospermia)
Prior vasectomy or failed vasectomy reversal
Problems with ejaculation
The procedures are usually done under local or general anesthesia. Most men feel only mild soreness or discomfort afterward, which resolves within a few days.
Yes. Sperm retrieval is generally safe when performed by experienced specialists. Risks such as swelling, mild pain, or temporary bruising are uncommon and usually short-lived.
No. Sperm obtained from these procedures are typically not motile enough for natural conception. They are directly used with ICSI (Intracytoplasmic Sperm Injection) during IVF.
Yes. If needed, sperm retrieval procedures can be repeated. In some cases, sperm can also be frozen and stored for future IVF/ICSI cycles.
No. The procedures do not usually impact hormone production or overall fertility, though your doctor will evaluate testicular function before and after the procedure.
Yes. Retrieved sperm is often frozen for future IVF or ICSI cycles.
No fertility treatment guarantees pregnancy, but sperm retrieval allows fertilization to occur when sperm is otherwise unavailable.
Success depends on the underlying condition and sperm production.